Transplant patients usually stay in the hospital 4–6 weeks or longer. Your child will stay in a special part of the hospital for transplant patients and other patients who have little or no immune system function. Infection control guidelines are different in the transplant unit than in other areas of the hospital.
Infusion of stem cells
The transplant process is challenging. But receiving the stem cells is relatively simple. It is much like a blood transfusion. Stem cells are in a bag or syringe connected through a tube to your child’s central line. It takes a few minutes to a few hours. It is not painful.
Engraftment
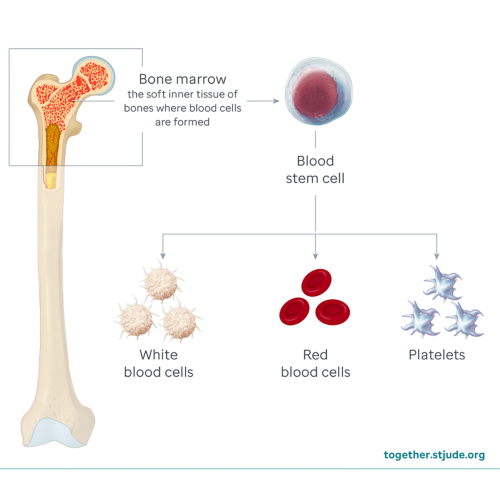
After entering the bloodstream, the stem cells travel to the bone marrow. Here they begin to divide. Stem cells become white blood cells, red blood cells, and platelets. This process is called engraftment.
Engraftment usually begins 2–4 weeks after you receive the cells. White blood cells are the first to engraft, followed by red blood cells, and then platelets. Your child may need transfusions of red blood cells and platelets to keep counts in a safe range while waiting for engraftment.
Doctors use blood tests to confirm that new blood cells are being made. After the transplant, your child will have daily blood draws for testing. Your care team will monitor your child’s red blood cells, white blood cells, and platelets to track the progress.
Bone marrow aspiration can also help doctors see how well the new stem cells are growing. This procedure involves the removal of a small sample of bone marrow through a needle for examination under a microscope.
Caring for your child
A parent or other adult family member will need to stay with your child in the hospital. The transplant process is physically and emotionally draining for caregivers. It is best to have more than 1 family caregiver who can care for your child. Each caregiver must be trained, so it is important to plan ahead.
Preventing infection
During the first part of the hospital stay, your child will have high-dose chemotherapy with or without radiation. The treatment makes room for the healthy stem cells and helps prevent rejection of donor cells. It also weakens the immune system, so your child will be at high-risk of getting an infection.
Patients and family caregivers must take many precautions to prevent infections, such as wearing a mask and washing hands often.
All visitors must be screened for possible infections and contagious illnesses. Every transplant center is different. Be aware of hospital rules for visitors.
General transplant unit guidelines include:
- All caregivers and visitors must meet certain screening criteria before entering the transplant unit and must follow infection control guidelines.
- Only the patient and family caregiver can stay overnight.
- Visiting hours are limited. The primary caregiver is not considered a visitor.
- The number of caregivers and visitors allowed in the room is usually limited.
- There may be age requirements for siblings and visitors.
- All caregivers and visitors must wash their hands when entering and leaving the patient’s room.
Supporting your child during transplant
Being away from family, friends, and normal activities can be hard. Your child’s care team will help your child be as comfortable as possible. Child life specialists can provide fun activities such as games and crafts. Rehabilitation therapists will create an exercise plan for your child and give ideas about how to stay active.
You can bring toys and other items to help your child feel more at home. Encourage your child to connect with others through texts, social media, video chats, e-mails, phone calls, and letters.
Keeping up with school
Your child will not be able to attend school during transplant and until their immune system has recovered. Your child can keep up with some schoolwork. Talk to your child’s school and connect with your hospital’s school services.