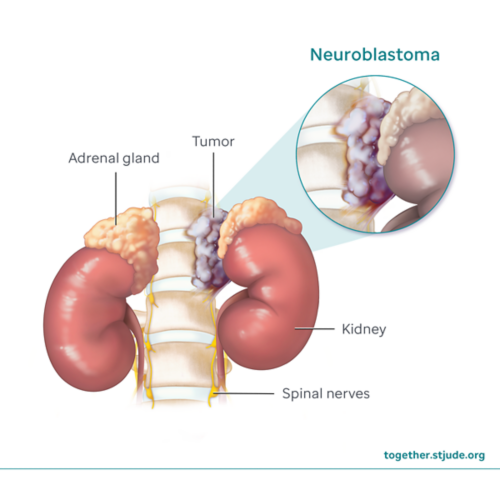
Neuroblastoma is a type of childhood cancer that grows from immature nerve cells (neuroblasts). It most often forms in the adrenal glands, small organs that sit on top of the kidneys. Neuroblastoma can also start in nerve cells in the abdomen, chest, neck, or pelvis.
Patients with neuroblastoma may have only one tumor, or the cancer may spread to other parts of the body (such as bone, bone marrow, liver, or skin).
Neuroblastoma is usually found in young children under age 5. About 750 children are diagnosed with neuroblastoma in the U.S. each year. It is the most common solid tumor in infants and young children outside the brain.
Treatments for neuroblastoma may include surgery, chemotherapy, bone marrow transplant, radiation therapy, immunotherapy, MIBG therapy, or a combination of treatments. Some neuroblastomas can be treated with surgery alone. Infants with low-risk neuroblastoma may be monitored without any surgery or treatment to see if the tumor goes away on its own. Neuroblastoma that has spread or come back after treatment needs more intensive therapy.
Symptoms of neuroblastoma
Signs and symptoms of neuroblastoma depend on where the cancer is located, the size of the tumor, and whether the cancer has spread. Over time, symptoms can become more noticeable as the tumor grows.
Neuroblastoma symptoms may include:
- Lump or mass in the abdomen (belly), chest, or neck
- Swelling or pain in the abdomen
- Bulging eyes or dark circles around the eyes (“raccoon eyes”)
- Changes in eye appearance or movement
- Loss of appetite
- Constipation or diarrhea
- Trouble peeing or pooping
- Back pain or bone pain
- Leg weakness or paralysis
- Irritability
- Feeling tired
- Fever
- High blood pressure
- Breathing problems
- Anemia (low red blood cells)
- Skin changes (such as lumps under the skin)
Horner syndrome
Some children with neuroblastoma develop Horner syndrome. This happens when the nerves that control the eyes and face on one side of the body are damaged. The main signs and symptoms of Horner syndrome are:
- Drooping eyelid
- Small pupil (black center of the eye)
- Lack of sweating on 1 side of the face
Risk factors for neuroblastoma
Neuroblastoma is most common in young children and usually occurs before 5 years of age. It rarely develops after age 10. Males have a slightly higher risk of developing neuroblastoma than females.
Sporadic neuroblastoma: In most cases, neuroblastoma happens without a family history, and the cause of neuroblastoma is unknown. This is called sporadic neuroblastoma.
Hereditary neuroblastoma: In 1–2% of cases (1 to 2 in 100 patients), neuroblastoma can be caused by an inherited gene change (mutation) passed down from a person’s parents. It is usually caused by a change in the ALK or PHOX2B gene found in all cells of the body (germline mutation).
Diagnosis of neuroblastoma
Neuroblastoma may not cause noticeable symptoms at first. The tumor may sometimes be found during a routine medical exam. In approximately 50% of patients, neuroblastoma spreads to other parts of the body before it is diagnosed.
Tests to diagnose neuroblastoma may include:
- Physical exam and health history to learn about symptoms, general health, past illness, and risk factors
- Blood tests to check blood counts and monitor kidney and liver function
- Urine tests to look for vanillylmandelic acid (VMA) and homovanillic acid (HVA). These substances are made by neuroblastoma tumor cells and are often higher than normal in children with this cancer.
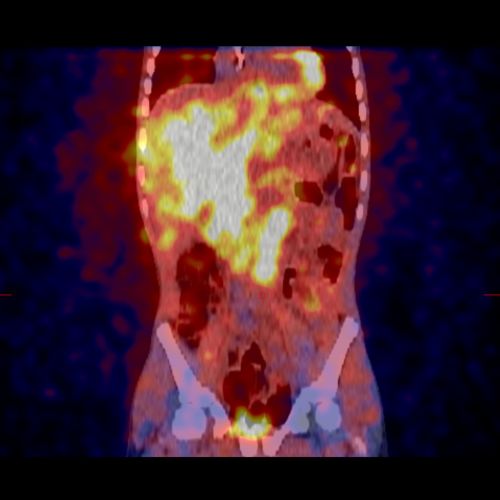
- Imaging tests such as ultrasound, CT, MRI, PET Scan, or MIBG scan to check the size and location of the tumor
- A neurological exam to measure how well the brain and nerves work. This includes tests of memory, vision, hearing, muscle strength, balance, coordination, and reflexes
- Bone marrow aspiration and biopsy to look at cells in the bone marrow and see whether cancer has spread
- Biopsy to remove a small piece of the tumor and look at the tissue under a microscope
- Genetic testing to find gene changes or mutations
Staging is used to describe the extent of cancer in the body. It is based on:
- Tumor location
- How the tumor affects nearby organs
- Spread of disease
Doctors stage neuroblastoma using the International Neuroblastoma Risk Group Staging System (INRGSS).
Neuroblastoma risk groups
Neuroblastoma can be grouped into 3 risk categories: low, intermediate, and high risk. These groups are based on:
- Child’s age: Patients under 18 months often have less aggressive disease.
- Stage of the disease: Neuroblastoma that has spread (metastatic) is harder to treat and higher risk.
- Tumor features: The way the tumor grows and its molecular and genetic features (biology). Tumors that have many copies of the MYCN gene (MYCN amplification) are considered high risk.
About half of neuroblastoma patients have high-risk disease. High-risk neuroblastoma means that the disease is:
- Harder to treat
- More likely to spread
- More likely to come back after treatment (relapse)
Your care team uses risk groups to plan the best treatment for neuroblastoma patients.
Treatment of neuroblastoma
Neuroblastoma treatment depends on the assigned risk group. Treatment options may include:
- Observation and close monitoring (no treatment)
- Surgery
- Chemotherapy
- High-dose chemotherapy with stem cell rescue (bone marrow transplant)
- Radiation therapy
- Immunotherapy
- MIBG therapy
Some patients may be eligible to be part of a clinical trial that tests new ways of treating neuroblastoma.
Prognosis for neuroblastoma
The chance of cure (prognosis) depends on several factors. These include:
- Child’s age
- Risk group
- Tumor features
- Whether the cancer has spread
- Tumor response to treatment
- If their cancer has relapsed (come back)
General survival rates based on risk groups:
- Low-risk neuroblastoma: about a 98% (98 in 100) chance of survival
- Intermediate-risk neuroblastoma: about a 95% (95 in 100) chance of survival
- High-risk neuroblastoma: less than 60% (60 in 100) chance of survival
Your child's doctor is the best source of information about your child's specific case.
Support for children with neuroblastoma
Patients need follow-up care (monitoring) to watch for the cancer coming back (relapse) after their treatment ends. The care team will tell you what tests are needed and when.
- In patients who do not have high-risk disease, the risk of relapse is 5–15% (5–15 in 100).
- In high-risk patients, the risk of relapse is about 50% (50 in 100).
Cancer is most likely to come back (relapse) within the first 2 years after treatment. Relapse is rare if there is no sign of cancer after 5 years.
Health after cancer
After completing treatment, it is important that your child:
- Have regular checkups and screenings by a primary care provider
- Maintain healthy habits, including physical activity and healthy eating
- Have a survivorship care plan to share with health care providers. This plan should include:
- Guidance on health screenings and medical care
- Disease risk factors
- How to improve health
Regular medical checkups by a primary health care provider are important to watch for health problems that can develop years after therapy. Survivors treated with chemotherapy or radiation should be monitored for long-term and late effects of therapy. Problems due to treatment could include:
Questions to ask your care team