The main treatment for medullary thyroid cancer is surgery to remove the thyroid gland. This is called a total thyroidectomy. The surgeon may also remove nearby lymph nodes and other tissues, known as neck dissection. These surgeries help stop the cancer from coming back.
An experienced surgeon should perform the surgery. Look for one who does this type of surgery regularly in pediatric patients. This lowers the risk of problems afterward.
The thyroid makes hormones that control some body functions. After thyroid removal, the body will not make these hormones. To replace the missing hormone, your child will need to take thyroid hormone replacement medication (levothyroxine) for the rest of their life. Physical therapy can help your child with neck strength and movement after surgery.
Preventive surgery for MEN syndromes
The best way to treat MTC is to prevent the spread of the disease. Children with genetic mutations are at higher risk for developing this cancer. Doctors may do surgery to remove the thyroid gland before cancer is found (prophylactic thyroidectomy).
Doctors recommend this surgery for children younger than 5 years who have a MEN2A mutation. A child with a MEN2B mutation should have a thyroidectomy before age 1. In patients with the MEN2B mutation, MTC develops early and is aggressive.
Risks of thyroid surgery
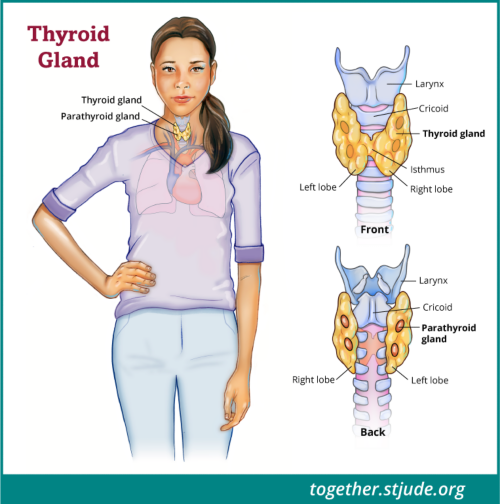
There is a risk of damage to neck structures during surgery, such as the nerves and parathyroid glands.
Hypoparathyroidism due to damage to parathyroid glands
Parathyroid glands are small and lie behind the thyroid. They keep calcium at normal levels in the body. Sometimes, parathyroid glands are harmed during surgery. The parathyroid glands may become "stunned" after this surgery, even if they are not damaged.
Patients may get a condition known as transient post-surgical hypoparathyroidism. Symptoms of this condition include:
- Low levels of calcium in the blood (hypocalcemia)
- Numbness and tingling in the hands, feet, and face
- Muscle cramps
Doctors treat this condition with vitamin D (calcitriol) and calcium supplements until these problems stop. Hypoparathyroidism may be brief or permanent.
Nerve or vocal cord problems
Another risk of thyroid surgery is nerve damage to the recurrent laryngeal nerve. This nerve helps the vocal cords move for speech. Nerve problems after thyroid removal are rare. The more experienced the surgeon, the lower the risk of problems. During the surgery, the surgeon may also use a special breathing tube to prevent injury to the nerves.
An otolaryngologist will do a "scope" procedure to check the vocal cords before and after surgery. The doctor will gently place a small, flexible camera into your child's nose to see the vocal cords and check their function.
Vocal cord injuries during surgery are often temporary. But some patients may need a longer recovery time, even a year or longer. Patients may need more treatment if their voice changes or they have problems breathing or swallowing.
The doctor can inject temporary material into the vocal cords to help them work better. In some cases, the patient may need surgery to improve vocal cord function.