Surgery to remove the thyroid gland (thyroidectomy) is the main treatment for thyroid cancer. This surgery:
- Lowers the risk of more thyroid cancer
- Helps with follow-up care using radioactive iodine for imaging and treatment
Before surgery, the care team will do an ultrasound and a fine-needle aspiration on any lymph nodes that may have cancer. This helps the doctor plan the surgery.
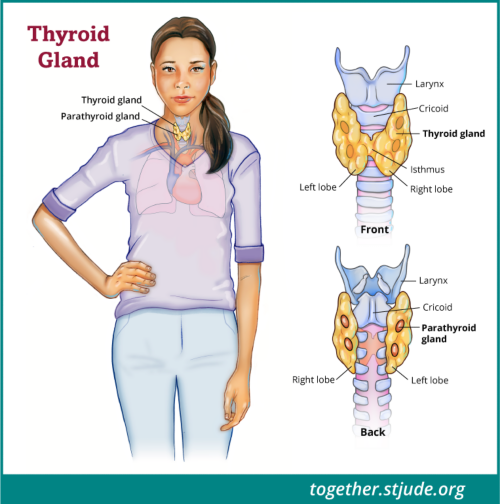
If the tumor is small, the surgeon may do a partial thyroidectomy. This procedure only removes 1 lobe and the isthmus of the thyroid gland. The isthmus is the thin band of tissue that connects the 2 lobes of the thyroid gland.
Your child's doctor may also remove lymph nodes and other tissues in the center or sides of the neck. This procedure is known as a neck dissection. The surgeon may remove lymph nodes that interact with the thyroid gland and may have cancer cells. High-risk patients may need more surgery to stop cancer from returning.
Risks of thyroid surgery
During thyroid surgery, there is a risk of damage to neck structures and parathyroid glands.
The parathyroid glands are 4 small glands that lie behind the thyroid. These glands release parathyroid hormone. This hormone keeps calcium levels at a normal level in the body.
Sometimes, the parathyroid glands are harmed during surgery. The parathyroid glands may become "stunned” even if they are not damaged. This results in hypoparathyroidism and low levels of parathyroid hormone.
Symptoms include:
- Low levels of calcium in the blood (hypocalcemia)
- Numbness and tingling in the hands, feet, and face
- Muscle cramps
Doctors treat this condition with vitamin D (calcitriol) and calcium supplements until these problems stop. Hypothyroidism may be temporary or permanent.
Nerve or vocal cord problems
Another risk of thyroid surgery is nerve damage to the recurrent laryngeal nerve. This nerve helps the vocal cords move for speech. Nerve problems after thyroid removal are rare.
A specialist will do a "scope" procedure to check the vocal cords before and after surgery. The doctor will gently place a small, flexible camera into your child's nose to see the vocal cords and check their function.
Vocal cord injuries during surgery are often temporary. But some patients may need a longer recovery time, even a year or longer.
Patients may need more treatment if their voice changes or they have problems breathing or swallowing. The doctor can inject a special filler into the vocal cords to help them work better while the nerve heals. This filler is made of safe materials that the body slowly absorbs over time. Sometimes, the patient may need surgery to improve vocal cord function.
After surgery, patients will have follow-up tests to decide if other treatments are also required.