Treatment of retinoblastoma depends on whether the tumor affects 1 eye or both eyes, the extent of disease, and whether the tumor has spread. Doctors also consider:
- The child’s age
- Family history and genetics
- Whether the tumor affects the center of vision
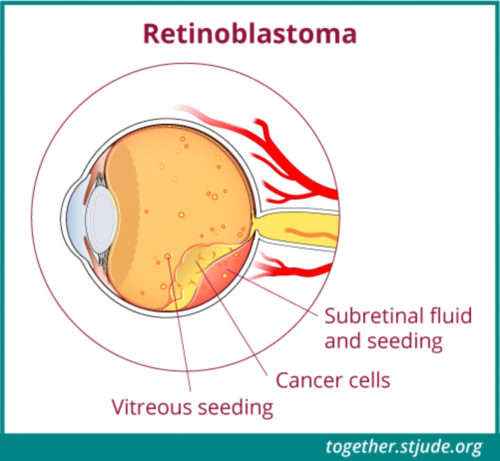
- Whether the tumor has broken apart into vitreous seeds
- Number of tumors
Treatments may include:
- Surgery
- Focal therapy
- Chemotherapy
- Radiation therapy
Usually, doctors use a combination of treatments. Before starting therapy, you should discuss the treatment plan with your child’s doctors to understand the short- and long-term risks and benefits.
Treatments for localized retinoblastoma
Chemotherapy
Chemotherapy, or chemo, uses strong medicines to kill cancer cells or stop them from growing. Chemo might use 1 medicine or more than 1 medicine.
Chemotherapy for retinoblastoma might include:
Chemotherapy alone cannot cure retinoblastoma. It is used along with other treatments.
Chemo for retinoblastoma might be given:
- Through the vein (intravenous)
- Near the eye (periocular)
- Directly in the eye (intravitreal)
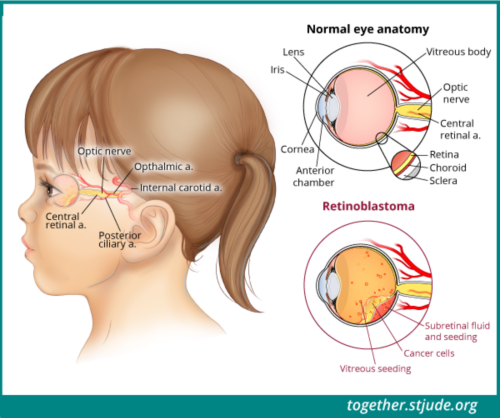
- Through the ophthalmic artery, either by ophthalmic artery chemosurgery (OAC) or intra-arterial chemotherapy
OAC should only be done by a medical team with experience in this technique to lower the risk of damage to the eye.
Focal therapy
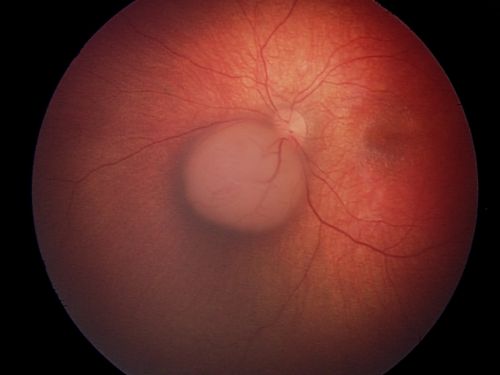
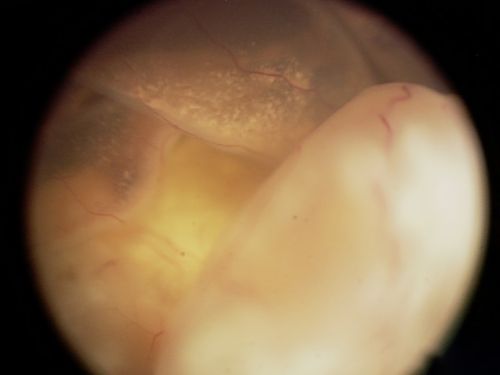
Focal therapy treats the tumor directly. If the tumor is very small, focal therapy alone may be enough to treat the cancer. It is done while the child is asleep under anesthesia. There are 3 types:
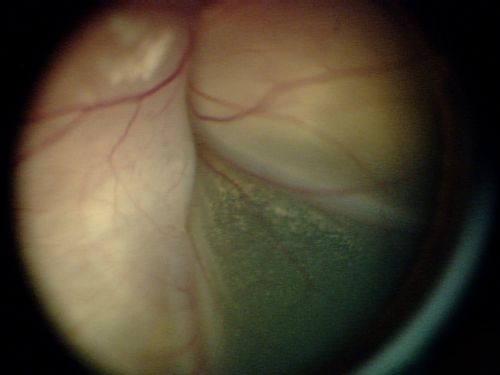
- Laser therapy: This therapy uses high intensity light or heat to kill cancer cells.
- Cryotherapy: This therapy uses freezing and thawing to shrink the tumor and kill the cancer cells.
- Plaque radiotherapy (brachytherapy): Surgeons place a small device made of radioactive material on the eye directly above the tumor. The device remains in place for a few days. Surgery with anesthesia is required to place and remove the device. After the device is removed, no radioactivity is left in the eye.
Surgery
Surgery is used to remove the eye if necessary. This surgery is called enucleation.
- Unilateral retinoblastoma: Most patients (70–90%) with only 1 affected eye do not need more treatment after the eye is removed. If the tumor has spread into tissues around the eye or eye socket, tests including bone marrow aspirates and biopsies and lumbar puncture are used to stage the disease. In these cases, patients need chemo because of a higher risk that the tumor will spread.
- Bilateral retinoblastoma: If 1 eye is removed, treatment focuses on saving the other eye. Doctors also consider the risk of tumor spread.
Radiation therapy
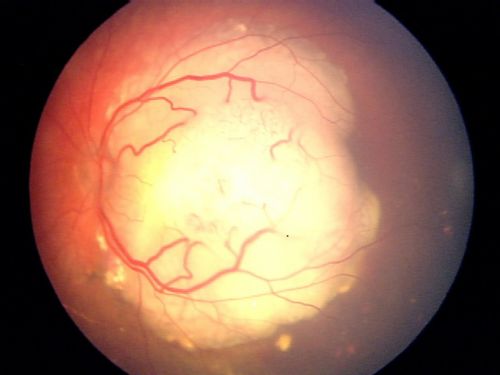
Radiation therapy may be used for advanced retinoblastoma. External beam radiation uses a machine to deliver radiation to the entire eye. This is the most aggressive treatment for retinoblastoma. It is used to help the child keep their vision and to prevent the cancer from spreading. Because of the risk of long-term effects and second cancers, radiation is usually only used for patients whose cancer:
- Has spread beyond the eye
- Has not responded to other therapies
- Has come back
Treatments for metastatic retinoblastoma
Very rarely, retinoblastoma spreads to the brain or cerebrospinal fluid. It can also spread to the liver, bones, bone marrow, or lymph nodes. Intensive chemo followed by autologous bone marrow transplant may be needed in these cases. Some patients may also need radiation therapy.