Melanoma is a type of skin cancer most often seen in adults. It also affects about 300–400 children and teens each year in the United States. Melanoma can develop on any part of the skin. It can also occur in the eye. If left untreated, melanoma can spread to other parts of the body.
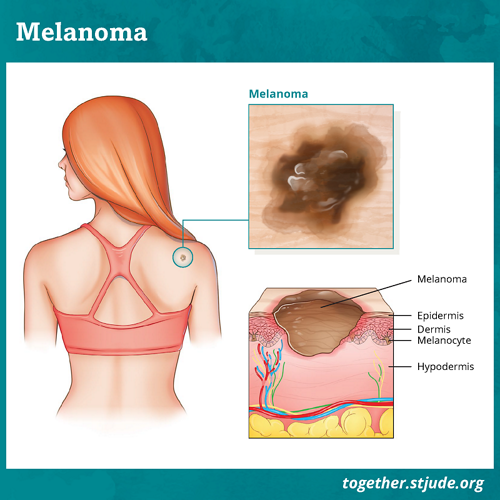
In melanoma, cancer forms in skin cells called melanocytes. These cells produce melanin, which provides color (pigment) to the skin.
Melanin helps protect the skin from ultraviolet radiation (UV radiation). People with darker skin have more melanin and are less likely to develop melanoma.
Melanoma accounts for about 1% of cancers in children under age 15. It occurs more often in older age groups.
Symptoms of melanoma include unusual skin changes such as:
- A mole that gets bigger, changes color, bleeds, or itches
- A pale or red-colored bump
Treatment for melanoma depends on the stage of disease. Patients usually have surgery to remove the cancer. More severe disease may require other treatment. This may include targeted therapy, chemotherapy and/or immunotherapy.
When caught early, survival rates for melanoma are good. But melanoma can spread to lymph nodes and other parts of the body. This can make it hard to treat. So, awareness and early detection of melanoma is quite important.
It is best to identify skin cancers as soon as possible. Skin cancer screening can help you do that.
Signs of melanoma include:
- A mole or bump on the skin that grows or changes shape, especially if changes occur in a short period of time
- An irregular-shaped or large mole
- A pale or red-colored bump on the skin
- A mole or bump that itches or bleeds
ABCDE method
A helpful way to think about signs of melanoma is to use the ABCDE method:
- A: Asymmetry – One half of the spot is different than the other.
- B: Border – The spot’s edges or border are notched or jagged, not smooth.
- C: Color variation – The spot’s color varies from one area to another.
- D: Diameter – Melanoma is often larger than a pencil eraser when diagnosed. But it could be smaller.
- E: Evolution – Melanoma’s shape, size, or color changes over time.
Risk factors for melanoma
Some factors increase the risk for melanoma. These include:
- Age – Melanoma is more common in teens than in young children.
- Skin color – People who have fair skin, light or red hair, light-colored eyes, and tend to sunburn easily are at higher risk. People with darker skin are less likely to develop melanoma.
- Skin conditions – People who are born with large, dark spots on their skin called melanocytic nevi are more likely to develop melanoma. Some inherited conditions can also increase risk. These include xeroderma pigmentosum, retinoblastoma, and Werner syndrome.
- Family history – Having a family history of melanoma or unusual moles increases melanoma risk.
- UV light exposure – UV radiation damages the DNA of skin cells. Sunlight is the main source of UV exposure. Tanning beds and UV nail-polish dryers are other sources. Learn how to protect your skin from sun and UV exposure.
- Sunburns – People with a history of blistering sunburns are more likely to develop melanoma.
- Radiation therapy – Patients who had radiation therapy have a higher risk of developing melanoma.
- Weakened immune system – Low immunity due to serious illness or transplant can increase melanoma risk.
Doctors use several procedures and tests to diagnose melanoma. These include:
- Health history and physical exam
- Skin exam
- Biopsy to collect tissue from deeper levels of the skin and see how far the tumor extends from the surface
- May want to add tests to see if there are genes that are abnormal in the melnoma like BRAF or others
Other tests may be needed if doctors think melanoma may have spread. These tests include:
- Blood tests – These may include checking the level of lactate dehydrogenase (LDH). The LDH level may be higher when melanoma is present.
- Lymph node mapping and a sentinel lymph node biopsy – These are used to see if melanoma has spread to nearby lymph nodes. Doctors inject a special dye or radioactive substance near the melanoma site. The dye travels through the lymphatic system to the lymph nodes closest to the original tumor. A surgeon can remove those lymph nodes and test them for cancer. This helps doctors find out the disease stage and plan treatments.
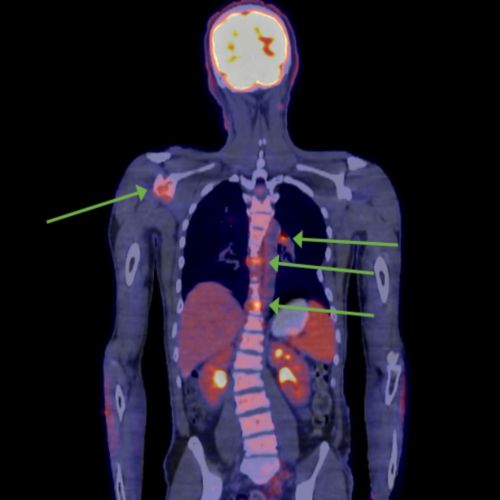
- Imaging tests – The type of tests depend on the specific tumor and the involvement of lymph nodes. Such tests may include magnetic resonance imaging (MRI), positron emission tomography (PET) scans, and computed tomography (CT or CAT scan).
Melanoma has several subtypes:
- Superficial spreading – The most common type of melanoma. It tends to grow slowly and appear more flat and broad.
- Spitzoid (spitz nevus) – The most common type of melanoma in younger patients. It looks like a mole.
- Nodular – Starts as a raised area that grows quickly, often deep into the skin.
- Lentigo maligna – A slow-growing type. It usually occurs on the head or neck of adults.
- Acral lentiginous – Most common in people with darker skin. It can occur on the soles of the feet, palms of the hand, and under nails.
Melanoma is classified in stages 1–4. These stages are based on factors that include:
- Tumor thickness or how deep melanoma is found in the skin
- If the tumor has cracked or broken through the top layer of the skin (ulcerated)
- If the tumor has spread to lymph nodes
- If the tumor has spread to other parts of the body
Treatment for melanoma depends on the:
- Location of the melanoma
- Features of the tumor (gene changes and histology)
- Stage of disease
The chance of recovery from melanoma depends on a variety of factors such as:
- Thickness of the tumor
- Location of the tumor
- If the cancer has spread to lymph nodes or other parts of the body and the number of areas it has spread to
- If surgery completely removes the tumor
- Level of lactate dehydrogenase (LDH) in the blood
Overall, the stage of disease is the most important factor for prognosis. Patients with melanoma that has not spread have an excellent prognosis. Survival rates are more than 90% in the United States. But patients whose disease has spread are more difficult to treat.
Late effects of treatment
Childhood cancer survivors should have long-term follow-up health care. Some treatments can cause late effects. These are health problems that happen months or years after treatment has ended.
It is important to have regular checkups and screenings by a primary health care provider. Your child should have a survivorship care plan after they complete treatment. It includes guidance on:
- Health screenings
- Disease risk factors
- How to improve health
Share this plan with your child’s care providers.
Survivors should adopt healthy habits to protect their health. This includes physical activity and healthy eating.