Mouth and throat sores are common side effects of cancer treatment in children. The clinical name for this condition is mucositis.
What is mucositis?
Mucositis is a swelling of the mucous membrane which is the moist, inner lining of some organs usually causing painful sores.
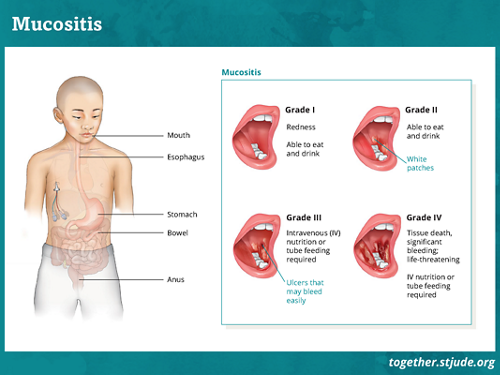
Mucositis can occur anywhere along the digestive tract including:
- Mouth
- Swallowing tube (esophagus)
- Stomach
- Intestines
- Anus
More than 50% of childhood cancer patients may develop mucositis. More than 75% of patients who have a stem cell transplant (also called a bone marrow transplant or hematopoietic cell transplant) may have this side effect.
What is oral mucositis?
Oral mucositis refers to mouth and throat sores. These are a cause for concern because they can:
- Cause pain and discomfort
- Make it difficult for patients to eat and drink
- Make patients more at risk for infection
- Cause changes to the patient’s treatment plan
Dealing with mouth and throat sores may include:
- Prevention
- Treatment of pain and discomfort
- Treatment of infections
- Nutrition support
Causes of mouth and throat sores
The factors that make patients more likely to develop mouth and throat sores include:
Signs and symptoms of mouth and throat sores
Patients and families should tell the care team when signs and symptoms appear.
Signs and symptoms include:
- Soreness or pain in or on the lips, mouth, or throat
- Difficulty swallowing
- Pain in the chest area following swallowing
- Increased discharge (drooling) from inside the mouth or throat
- White patches or sores in the mouth or throat
- Bleeding from gums
- Body temperature above 100.4 F or 38.0 C
Diagnosis of mouth and throat sores
The care team diagnoses mouth and throat sores by:
- Physical exam of the mouth and throat
- Patient’s report of pain and inability to eat and drink
The care team will grade the oral mucositis from 1-4 based on how bad it is. This grade will help guide the treatment. Grades 3-4 are severe. Complications are more likely.
Prevention of mouth and throat sores
Mouth and throat sores cannot be prevented in some cases. But there are steps patients can take to possibly lessen the severity of the symptoms.
- Dental exam — If possible, your child should have a dental exam before treatment begins. Make sure the dentist knows your child is a cancer patient. You may need to remove oral appliances or braces before treatment begins.
- Daily mouth care (oral hygiene) — Follow the care team’s instructions even if oral care is painful.
- Brush teeth gently with a soft toothbrush. Tooth brushing can cause gums to bleed and provide a way for harmful bacteria to enter the bloodstream. Ask your care team about oral swabs or sponges if tooth brushing is not possible.
- Only use mouth rinses recommended by the care team. Antibacterial rinses such as chlorhexidine can remove bacteria from the mouth.
- Flossing may not be possible. Ask the care team before flossing. It can damage tissue and cause bleeding and infection.
- A dietician may recommend a soft diet at the beginning of chemotherapy to prevent cuts in the mouth.
- Foods that are easy to chew and swallow
- Foods that do not have a rough texture
- Foods that aren’t spicy
- Foods and drinks that aren’t acidic
- Foods and drinks that aren’t very hot or cold
- Drinks that aren’t carbonated
- Dry mouth prevention — The care team may encourage ways of preventing dry mouth. These methods may include:
- Using a saliva substitute or mouth rinse
- Consuming sugar-free candy and gum
- Lip care — Use lip moisturizers recommended by the care team.
- Ice therapy — Eating ice chips before and during short periods of chemotherapy may slow the development of mouth sores. This process is called cryotherapy for mouth sores.
- Palifermin — Doctors sometimes recommend a medicine called palifermin to patients receiving autologous stem cell transplant.
Low-level laser therapy is under study as a prevention and treatment method.
It uses light to:
- Promote tissue regrowth
- Reduce inflammation
- Reduce swelling
- Relieve pain
Treatment of mouth sores
Treatment focuses on lessening pain, treating infections, and making sure the patient gets the necessary nutrition.
Pain management
Pain treatments will depend on the patient’s symptoms.
They may include:
- Rinses or “magic mouthwash” — The care team may recommend certain rinses or a “magic mouthwash” solution. They can soothe pain, fight infection, and reduce swelling.
- Topical gels — Gels recommended by the care team may soothe discomfort.
Other treatments may include different types of pain medications. The care team may encourage other forms of pain treatment that do not include medication.
Nutrition support
Patients can become dehydrated or malnourished when they have problems eating and drinking.
They may need to receive nutrition through tube feeding or total parenteral nutrition (TPN).
Treatment for infections
Mouth and throat sores provide a place for germs to enter the body and may lead to infection.
Treatment of infection may include medicine to treat infection. The care team may work with others to find the best infection treatment plan.