What is a blood transfusion?
A blood transfusion is a procedure that gives whole blood or blood products (parts of blood) to a patient through a vein. Your child may need a blood transfusion if their body cannot make enough blood cells.
Blood cells develop in the bone marrow, which lies in the center of the bones. Some diseases and treatments can affect the blood or bone marrow and reduce the number of blood cells. These include:
Your child may need 1 or more transfusions to treat a specific medical problem. Or your child may need repeated (chronic) transfusions over time to prevent moderate to severe health problems caused by a disease.
Blood is made up of several parts. These are separated from the blood to make blood products. Parts of blood include:
- Red blood cells have an iron-rich protein called hemoglobin. Hemoglobin carries oxygen from the lungs to the body's organs and tissues. Red blood cells also help the body get rid of waste products.
- Platelets prevent bleeding by helping the blood to clot.
- White blood cells fight infections and protect against germs.
- Plasma is the blood's liquid part. It contains water, proteins, and substances that help blood clot.
Types of blood transfusions
Blood is usually separated into parts, so your child only gets the blood products they need. The blood cells may come from a donor or from the patient.
Red blood cell transfusion
If your child has anemia or a decrease in red blood cells, they may need this type of transfusion. Your child may also need red blood cells if they do not have enough hemoglobin to carry oxygen through their body.
Platelet transfusion
Your child may need this type of transfusion if they have low platelet counts, a condition known as thrombocytopenia. A platelet transfusion can help prevent or treat bleeding.
White blood cell transfusion (granulocyte transfusion)
Your child may need this transfusion if they have a severe infection that does not improve with antibiotics. Granulocytes are the type of white blood cell that is transfused.
Plasma transfusion
If your child bleeds too much, your health care provider may order a plasma transfusion. Plasma has proteins called coagulation factors that help blood clot and stop bleeding.
Red blood cell and platelet transfusions are the most common types of blood product transfusion.
What to expect before a blood transfusion
Before a blood transfusion, your child may have blood tests to check their blood type and to look for antibodies in their blood.
- Blood type: There are 4 main blood groups: A, B, AB, and O. Blood can also have a protein called the Rh factor, which can be present (Rh positive or +) or absent (Rh negative or -). Based on the results, your child’s blood type may be A+, A-, B+, B-, AB+, AB-, O+, or O-. Knowing your child’s blood type is important for matching them with compatible blood products.
- Antibodies: Antibodies are proteins that are made by the immune system to help the body recognize and fight foreign substances. In some cases, antibodies in your child’s blood can attack donor blood cells.
Testing for blood type and antibodies helps ensure that the transfusion is safe and uses blood products that are right for your child.
Type and screen test
A type and screen is a blood test that determines your child’s blood type and screens for antibodies. During treatment, some people develop antibodies in their blood. Any antibodies will be detected by the type and screen test. If certain antibodies are found, specific blood products must be used.
A type and screen test is only valid for 3 days after it is collected.
ABO verification
ABO verification is a blood test needed to verify your child’s blood type. The first time your child needs a transfusion, this test will be done twice to make sure the blood type is correct.
What to expect during a blood transfusion
Most blood transfusions are done in a hospital setting, often in the infusion center, during surgery, or at a patient's bedside.
Before some transfusions, a blood test is done to check your child’s blood type. This is known as a “type and screen.”
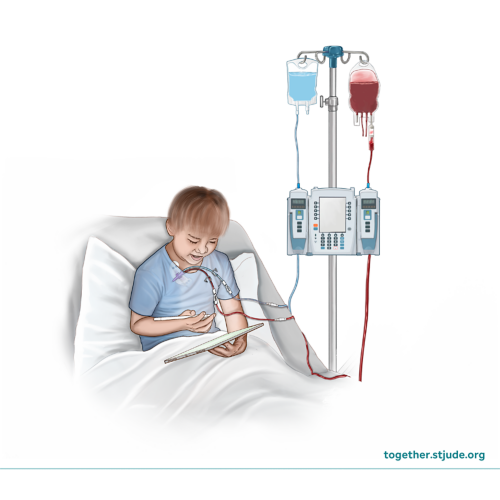
During a transfusion, your child will get blood cells through a small tube (catheter) that travels to a vein in their body. The time needed for the transfusion depends on the type of transfusion, the amount of blood product, and how much your child weighs.
When it is time for your child's transfusion:
- The nurse will check your child's vital signs including blood pressure, heart rate and body temperature.
- Staff will check the blood product to make sure it is correct.
- If your child has a central line (catheter), they may get the transfusion through the device. If not, your child will get it through a vein by IV.
- The nurse will connect the blood product bag to an IV pump, which controls the flow of blood product.
- Staff will carefully watch your child to see if they have any symptoms of a reaction to the blood product.
- The nurse will recheck your child's vital signs during and after the transfusion.
- If your child has an IV, the nurse will remove it.
- The nurse will talk to you about signs and symptoms to watch for and how to care for your child after the transfusion.
Risks of blood transfusions
In most cases, any side effects are usually mild and temporary. There is always the risk of rare or unknown side effects.
Contracting a disease or infection can occur through blood transfusion, but it is rare. Safety steps are in place to screen blood donors to make sure they are healthy. Donated blood is tested extensively before a patient gets a transfusion.
Blood transfusion reaction
Some patients may have reactions to transfusions. Typically, these cause mild symptoms, such as fever or a skin rash. In rare cases, a reaction may be severe. In some cases, the reaction can be treated, and the transfusion can continue. In other cases, the care team will stop the transfusion.
Symptoms of a blood transfusion reaction can include:
- Fever
- Chills
- Skin rash, itching, hives
- Flushing skin
- Swelling in the face, near the eyes and mouth
- Trouble breathing
- Nausea or vomiting
- Dizziness or fainting
- Changes in pulse or blood pressure
Hemolytic transfusion reaction
A patient must receive a blood product that works with their blood type. If the blood product is not correctly matched to the patient’s blood type, the body can attack the donor blood and make the patient sick.
In rare cases, a severe hemolytic transfusion reaction may occur. This reaction happens when the donated product does not match or work with the patient's blood type. The patient’s body attacks the transfused blood cells, which release substances that can harm the kidneys. The transfusion will stop at the first sign of this reaction.
Symptoms of a hemolytic reaction include:
- Fever
- Chills
- Back pain
- Flank pain
- Low blood pressure
- Dark urine
Blood products are most often donated by volunteer blood donors. Sometimes a friend or family member donates blood for a specific patient. In some cases, the patient’s own blood can be used.
Blood banks take steps to make sure that blood is safe:
- Potential blood donors are asked questions about risk factors that could affect the safety of the donated blood. They are not allowed to donate if risk factors are found.
- Blood banks type and match blood products to make sure they are compatible with the patient’s blood.
- Donated blood is tested for several types of infections. If the blood is positive for any of these infections, the blood is not used.
- Blood may also be screened for certain antibodies.
If you have questions about blood transfusions, including the risks and benefits, talk to your care team.