What is CAR T-cell therapy?
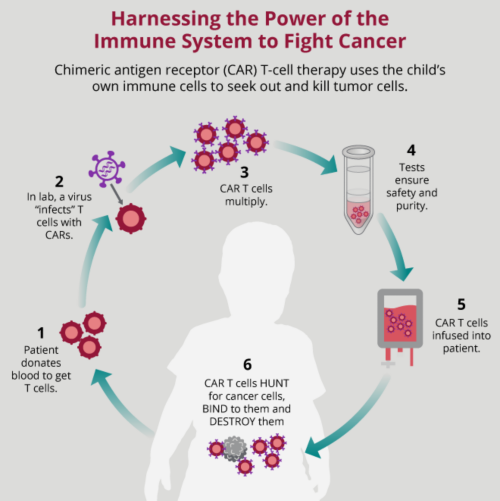
CAR T-cell therapy is a type of immunotherapy that works by using your body’s immune system to fight cancer cells.
Your immune system includes several types of cells. T cells, a type of white blood cell, are one of these immune cells. They look for abnormal cells. If T cells find one of these abnormal cells, they destroy it.
Cancer cells are abnormal cells that your body’s T cells did not destroy. That is where CAR T-cell therapy can help. CAR is short for chimeric antigen receptor, a certain type of receptor made in a lab that binds to proteins on cancer cells.
How CAR T-cell therapy works
CAR T-cell therapy can make your body better at fighting cancer cells. The therapy encourages your body’s T cells to recognize specific cancer markers, helping the T cell to see the cancer cell as abnormal and destroy it.
Your body creates cancer markers in response to cancer cells. Or the cancer cells themselves may make markers. Cancer markers are different substances in blood, urine, and other tissues.
The therapy allows your body’s immune system to locate and kill cancer cells.
Cancers CAR T-cell therapy can treat
Currently, doctors use CAR T-cell therapies to treat:
- Certain types of relapsed leukemia or leukemia that has not responded to treatment
- Certain types of relapsed lymphoma or lymphoma that has not responded to treatment
Scientists are studying how CAR T-cell therapy could be used to treat solid tumors and brain tumors, as well as other illnesses such as HIV.
What to expect in CAR T-cell therapy
Collecting T cells
CAR T-cell therapy starts by collecting T cells from the blood. This process is called apheresis. Your child’s appointment could be at the hospital. Or it might be at a blood donor center.
Before your child’s apheresis appointment, they may need certain medicines to prevent blood clots. They may also need to stop taking NSAIDs such as ibuprofen or aspirin. Listen carefully to any medication instructions from the care team and follow them.
During your child’s appointment, a member of the care team will place an IV in both arms. One of these IVs will allow blood to flow out. The other will let blood flow back in after a machine collects and stores the white blood cells.
If your child has a central line, your child’s care team might use it instead of an IV. Some children may need a temporary central line.
Apheresis usually takes 3–6 hours. Afterward, a member of the care team will count the cells to ensure there are enough. This process usually takes 1–2 hours. Your child may need another appointment if there are not enough cells collected.
Side effects after T-cell collection
Your child might have some side effects after apheresis and the anti-clotting medications they receive. Side effects may include:
- Bleeding
- Bruising
- Dizziness and fainting
- Feeling anxious or cold
- Nausea
- Numbness or tingling
- Muscle cramps
Anti-clotting medicine can also affect the way your child’s body uses calcium. If this happens, your child may be given calcium to help with side effects.
Apheresis can lower the number of red blood cells and platelets. Your child might need extra blood through a blood transfusion if this happens.
Manufacturing CAR T cells
CAR T-cell therapy is personalized. It can take 2–3 weeks to make your child’s T cells into the CAR T cells. This process is called manufacturing the CAR T-cells. Making the CAR-T cells does not always work. If this happens during your child’s CAR T-cell therapy process, it is not their fault.
While your child is waiting for therapy, they might still need other treatments such as chemotherapy, radiation, or surgery. Talk with your child’s care team. Follow any directions they give you exactly.
CAR T-cell infusion
Before your child’s CAR T-cell infusion, they may need a few days of lymphodepleting chemotherapy. This will temporarily decrease your child’s immune cells so that the CAR T cells are better able to grow and fight.
After your child’s CAR T cells are manufactured and they have any necessary chemotherapy, they will have an infusion of the cells. This process is like a blood transfusion. The CAR T cells are given through an IV or a central line.
It is not a painful process. It can take a few minutes or a few hours.
If the infusion goes as planned, these new cancer-fighting T cells continue to multiply in your child’s body. They will recognize, target, and kill the cancer cells.
CAR T-cell infusion side effects
Follow your care team’s instructions and make sure your child takes any medicines as prescribed after CAR T-cell therapy. CAR T-cell therapy can be very effective. But there are serious potential side effects.
Cytokine release syndrome (CRS) is one of the most serious side effects after CAR T-cell therapy. It can happen after the T cells are activated and release cytokines into the body. It most commonly begins 3–14 days after the infusion.
Symptoms of cytokine release syndrome may include:
- Fever
- Low blood pressure
- Low oxygen
- Dizziness and decreased coordination
- Headache
- Joint or muscle aches
- Nausea
- Vomiting
If your child begins to run a fever after CAR T-cell therapy, contact your care team immediately.
Other side effects can include allergic reactions, weakened immunity, and low blood cell counts. Reach out to your child’s care team if you have questions about side effects.
Patient safety information
For patients receiving tisagenlecleucel (KYMRIAH):
- You will be given a Patient Wallet Card with information on the side effects of CAR T-cell therapy. Keep this card with you at all times.
- You must stay within 2 hours of the hospital for at least 4 weeks after receiving KYMRIAH, unless otherwise indicated by your doctor.
- Do not drive or do hazardous activities or jobs (such as operating heavy or potentially dangerous machinery) for at least 8 weeks after receiving KYMRIAH.
Always follow the instructions given by your care team. Talk to your doctor or pharmacist if you have questions or concerns.