What is hemolytic anemia?
Causes of hemolytic anemia
Intrinsic or inherited hemolytic anemias
Most hemolytic anemias are caused by inherited conditions. This means the disorder is passed down from parent to child. But your child could be the first person in the family to have the condition. Your child might pass it on to their children.
Inherited conditions that lead to hemolytic anemia include:
- Hemoglobin disorders: These conditions include sickle cell disease, thalassemia, and hemoglobin C disease. Hemoglobin is a protein in red blood cells that carries oxygen. In these disorders, your child’s body does not make hemoglobinnormally and red blood cells break down sooner than they should.
- Membrane disorders: These disorders include spherocytosis and elliptocytosis. The red blood cells have an abnormal cell membrane. This causes them to be a different shape and be easily damaged.
- Enzyme deficiencies: These include G6PD deficiency and pyruvate kinase deficiency. In these conditions, an enzyme that helps protect red blood cells is missing causing. The missing enzymes cause red blood cells to break down more easily.
Extrinsic or acquired hemolytic anemia
Hemolytic anemia can also be caused by conditions that develop later in life and harm healthy red blood cells. These include:
Diagnosis of hemolytic anemia
Hemolytic anemia is diagnosed based on your child’s medical history, physical exam, and lab tests. Your child’s doctor may refer you to a hematologist, a doctor who diagnoses and treats blood disorders.
Lab tests may include:
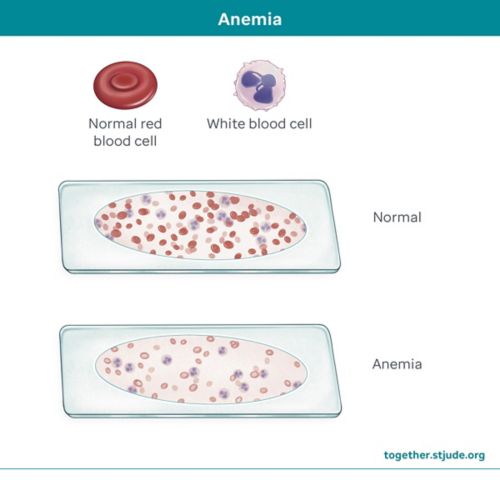
- Complete blood count (CBC) to look for signs of anemia. A CBC test measures:
- The number of red blood cells, white blood cells, and platelets
- The size of red blood cells
- Hematocrit, which shows how much of the blood is made up of red blood cells
- Hemoglobin, a protein in your blood that carries oxygen
- Peripheral blood smear to look at blood cells under a microscope
- Reticulocyte count to measure the number of young red blood cells in your child’s body. A high reticulocyte count means the bone marrow has to make more cells to replace damaged ones.
- Bilirubin test to measure bilirubin levels. Bilirubin is a substance made by the liver when red blood cells are broken down.
- Direct antiglobulin test (Coombs test) to see if the body is making antibodies against red blood cells
- Haptoglobin test to measure haptoglobin, a protein that gets rid of substances made by damaged red blood cells. Your child will have low levels if their body is using haptoglobin for this purpose.
- Urine tests to check for hemoglobin and iron in urine (pee)
Your care provider may order more tests to determine the type of anemia and its cause.
Treatment of hemolytic anemia
The right treatment for your child depends on the cause and severity of hemolytic anemia and your child’s medical needs. If the condition is not severe, your child may not need treatment and instead be closely monitored through regular blood tests. If anemia is linked to another condition, it is important to identify and treat the underlying cause.
Treatments to manage or treat hemolytic anemia include:
- Blood transfusions to replace red blood cells
- Medicines to help your child’s body make more red blood cells or to keep the immune system from attacking stem cells
- Surgery to remove the spleen (splenectomy). A splenectomy can reduce the number of red blood cells that are removed from the body.
- Surgery to remove the gall bladder. Some children with hemolytic anemia develop gallstones. They might need their gallbladder removed by surgery if the stones cause abdominal pain or other symptoms.
- A stem cell (bone marrow) transplant to replace damaged blood-forming stem cells with healthy stem cells from a donor. A transplant is very rarely used for hemolytic anemia.
Prognosis for hemolytic anemia
The prognosis for hemolytic anemia depends on the type of anemia and its cause. Most children with hemolytic anemia do well. Severe hemolytic anemia that is not treated or managed can cause irregular heart rhythms, an enlarged heart (heart that is larger than normal), and heart failure.
When to call your care team
Contact your child’s care team if your child:
- Looks pale
- Has increased yellowing of the skin
- Has dark urine
- Is more tired than usual
Talk to your care team about any questions or concerns you may have.
Questions to ask your care team