The right treatment for your child depends on the severity of symptoms and your child’s medical needs. It is important that your child has regular medical care and monitoring, including blood counts, bone marrow tests, and screening for cancer and other problems.
Fanconi anemia treatment can include short-term and long-term treatment strategies to address complications and improve quality of life.
Treatments for Fanconi anemia include:
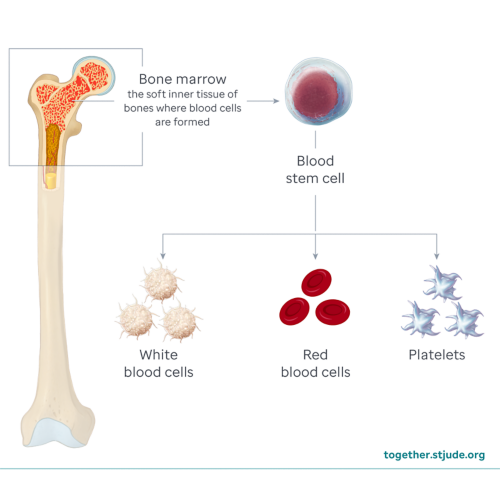
Stem cell (bone marrow) transplant
A bone marrow transplant is the only long-term treatment for bone marrow failure caused by Fanconi anemia. Healthy bone marrow from a donor (allogeneic transplant) replaces damaged bone marrow.
For a successful bone marrow transplant, an HLA-matched donor is needed. HLA (human leukocyte antigens) are proteins on cell surfaces. Doctors need to carefully match these markers between the donor and patient to prevent dangerous immune system reactions and transplant rejection. A transplant is not an easy process and can have complications including immune system reaction, rejection of donor cells, or infection. Even with a transplant, your child can be at risk for other health problems and complications of Fanconi anemia.
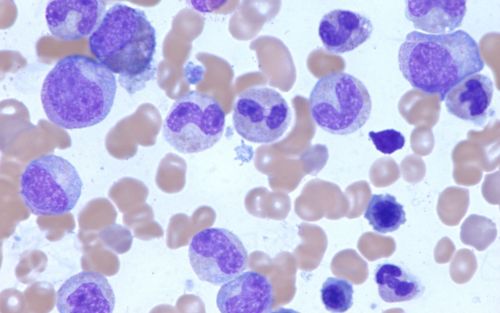
Blood transfusions
Your child may receive transfusions of red blood cells or platelets from a healthy donor. This can help treat symptoms but is not a cure.
Androgen therapy
Androgens (male hormones) can help the body make more red blood cells and platelets. Androgen therapy can temporarily improve blood cell production in some patients. It can help manage symptoms, but your child will need regular monitoring for side effects.
Growth factor medicines
In some rare situations, growth factor medicines such as eltrombopag or filgrastim (G-CSF) can be used to boost stem cell production to help the body make more blood cells.
Treatments to prevent or manage infections
Patients with Fanconi anemia can have very low white blood cell counts and are at high risk for life-threatening infections.
- Antibiotics, antivirals, and antifungals: To treat or prevent infection, your child may need medicines to kill bacteria (antibiotic), viruses (antiviral), or fungi (antifungal).
- Vaccinations: Staying up to date with vaccines can help prevent infections, especially if your child has a weak immune system due to low blood counts.
Surgery
Some children may need surgery to treat complications of Fanconi anemia such as physical abnormalities, tumors, heart defects, kidney problems, or other organ problems.
Gene therapy
Scientists are studying new gene therapy treatments that work by repairing faulty genes in a patient’s stem cells. These therapies are new but may be offered through a clinical trial in the future.