What is adrenocortical tumor?
Adrenocortical tumor (ACT) is a rare tumor of the adrenal gland. These tumors can be benign or malignant. You might also hear ACT called:
- Adrenocortical cancer
- Cancer of the adrenal cortex
- Adrenocortical adenoma
- Adrenocortical carcinoma
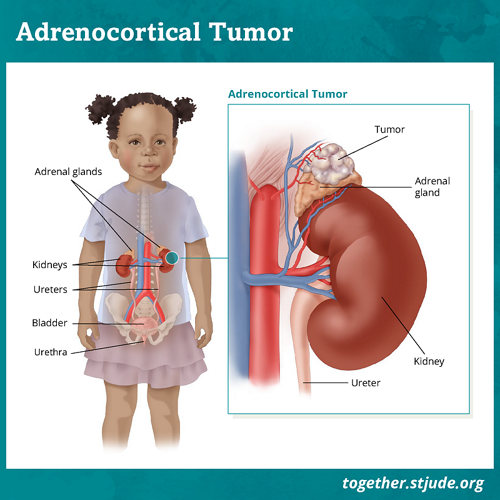
The body has 2 adrenal glands, 1 on top of each kidney. The adrenal glands produce hormones such as cortisol and aldosterone. These hormones have important jobs such as:
- Controlling how the body uses carbs, fats, and proteins for energy
- Helping the body cope with stress
- Controlling blood pressure
- Regulating water, potassium, and salt in the body
The outer layer of the adrenal gland is called the adrenal cortex. The adrenal cortex produces male and female sex hormones called androgens and estrogens. These hormones affect the development of male and female traits.
ACT treatment usually includes surgery to remove the tumor and adrenal gland. There is a good chance of cure if the tumor is fully removed by surgery. If the cancer spreads beyond the adrenal gland, then treatment includes chemotherapy. ACT is rare in children. It makes up only 0.2% of childhood cancers. The U.S. has about 25 new cases each year.
Symptoms of adrenocortical tumors
Most children with ACT show signs due to excess hormones. If cancer causes the adrenal glands to make more hormones than normal, this is called “functioning ACT.” In children, 90% of adrenocortical tumors are functioning. In teens, about half are functioning.
Signs of ACT depend on the hormones affected:
Androgens
In childhood ACT, most tumors release high numbers of male sex hormones. In boys, this may cause early puberty. Signs include:
- More facial and body hair
- Early pubic or underarm hair
- Body odor
- Acne
- Deepening voice
In females, extra androgens can cause growth of facial and body hair and deepening voice. Older girls may stop having their monthly period.
Estrogens
If too many female hormones are produced, girls can show early signs of puberty. Breasts may develop. Rarely, periods may start. Extra estrogen in boys may cause breast tissue to grow.
Cortisol
Cortisol comes from the cortex of the adrenal gland. This hormone helps control the body’s stress response. Adrenocortical tumors can cause too much cortisol to be produced. This condition is called Cushing syndrome. Signs include:
- Weight gain
- Rounded face
- Hump on the upper back
- Stretch marks
- High blood sugar
- High blood pressure
Aldosterone
Aldosterone is important for kidney function. It helps to balance water, salt, and potassium in the body. Adrenocortical tumors can produce excess aldosterone. This can cause:
- High blood pressure
- Thirst
- Weakness
- Muscle cramps
Other symptoms of ACT include:
- Lump or swelling in the belly
- Pain in the belly or back
- A feeling of fullness if the tumor presses on the stomach
Risk factors and causes of adrenocorticol tumor
Adrenocortical tumors are more common in girls than boys. ACT occurs most often in children ages 1–4.
ACT may be passed down in families (inherited).
Genetic predisposition and ACT
Inherited syndromes that increase ACT risk include Li-Fraumeni Syndrome (TP53 gene) and Beckwith-Wiedemann syndrome. Children with these conditions need regular screening for ACT.
Diagnosis of adrenocortical tumors
Doctors look for adrenocortical tumors in several ways. These include:
Doctors use several tests to diagnose ACT. Tests may include:
- Physical exam and health history
- Blood and urine tests to check adrenal hormone levels
- Imaging tests to learn about the size and location of the tumor, such as:
After surgery to remove the adrenal gland, doctors will study tissue from the tumor for signs of cancer. A biopsy is not usually done before surgery.
Staging of adrenocortical tumor
The stage of ACT depends on several factors:
- Tumor size
- Whether the tumor can be fully removed with surgery
- Whether the tumor has spread
In more than half of ACT patients, the tumor has spread by the time it is diagnosed. The most common places for the disease to spread are the liver and lungs. ACT may also spread to lymph nodes, bones, or within the abdomen.
Treatment of adrenocorticol tumors
Hormone monitoring and therapy can help patients with abnormal hormone levels due to the tumor or treatment. Medicines may help relieve some of these problems.
Patients may need hormone replacement therapy after surgery or treatment. Low adrenal hormones can affect the body's ability to regulate blood pressure and blood sugar.
ACT is a complex disease. A team that includes different types of providers is important. This team may include:
- Pediatric oncology
- Diagnostic imaging
- Surgery
- Pathology
- Radiation oncology
- Endocrinology
- Pediatric psychology
- Nutrition
- Genetic counseling
ACT patients ages 21 and younger are invited to take part in a registry to study this rare cancer:
Prognosis for adrenocortical tumor
Recovery from ACT depends on whether surgery removes the tumor. Chance of survival is higher with full removal of cancer by surgery.
If ACT is caught early and surgery is successful, the 5-year survival rate is 85%. For advanced cancer, the survival rate is less than 40%. Survival rates are only estimates. Your child’s doctor is the best source of information on the survival rate for your child.
All ACT patients need long-term monitoring and follow-up health care.
These factors can affect chance of cure:
- Tumor size
- Whether surgery fully removes the cancer
- Patient’s age (prognosis is better in children under age 3)
- Histological features (features seen under a microscope)
- Whether the cancer has spread
- Gene changes in the tumor
Support for patients with adrenocortical tumor
Children with ACT need ongoing care to check hormone levels and watch for cancer coming back.
Endocrine function monitoring
It is important to monitor endocrine function in patients with ACT. Children with functioning tumors need medicines to treat symptoms of excess hormones. Children with low adrenal gland function need hormones to help regulate the body’s functions, including the stress response.
Genetic testing and counseling
Children with ACT should be tested for the TP53 gene. People with a germline mutation in this gene have a condition called Li-Fraumeni syndrome. Family members of patients with this mutation should also be tested.
The TP53 gene is found in cells throughout the body. It tells cells to make a protein that keeps bad or damaged cells from dividing.
A change in TP53 raises the risk for certain cancers. People with a mutation in this gene should avoid exposure to radiation. Lifelong monitoring is important because of high cancer risk.
Late effects of adrenocortical tumor therapy
Childhood cancer survivors should receive long-term follow-up care. Some treatments can cause late effects. These are health problems that happen months or years after treatment has ended.
It is important to have regular checkups and screenings by a primary health care provider. Your child's care team should give you a survivorship care plan after treatment has ended. This report will include needed tests and tips for a healthful lifestyle. Your child should share this plan with their health care providers.
For general health and disease prevention, cancer survivors should adopt healthy habits to protect their health including physical activity and healthy eating.