NovoLog® (NŌ-vō-log) FlexPen® allows you to give your child insulin without having to get medicine out of a vial with a separate syringe.
The NovoLog FlexPen contains insulin aspart (AS-part), also called NovoLog, which is a rapid-acting insulin.
- It is used to help patients with high blood sugar levels.
- It is a clear, colorless liquid that is injected under the skin.
- NovoLog starts acting very fast.
- It may be prescribed by your doctor to take before meals or as a correction dose for a high blood sugar level.
The NovoLog FlexPen can be taken almost anywhere. You can fit it in your pocket or purse.
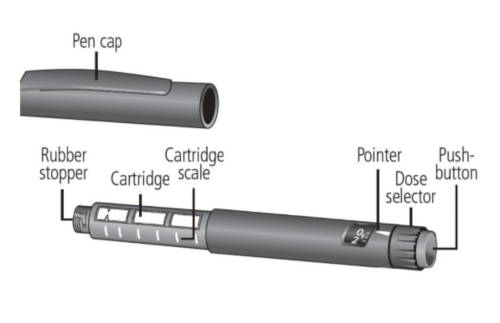
The NovoLog FlexPen
NovoLog FlexPen is a prefilled disposable device that looks like a pen. It contains 300 units of U-100 NovoLog insulin.
NovoLog FlexPen can deliver doses from 1 to 60 units in a single injection. The large dose display shows the number of units you have selected to give as a single dose.
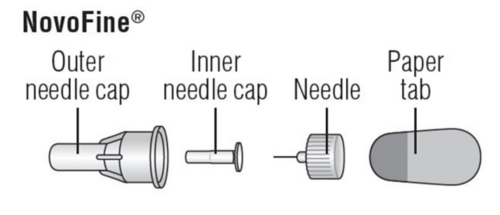
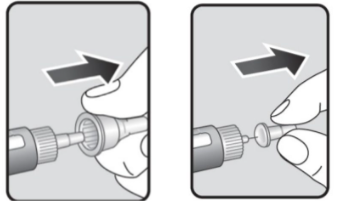
Needles for the NovoLog FlexPen
You will receive needles made specifically for the NovoLog FlexPen. These are called NovoFine® needles.
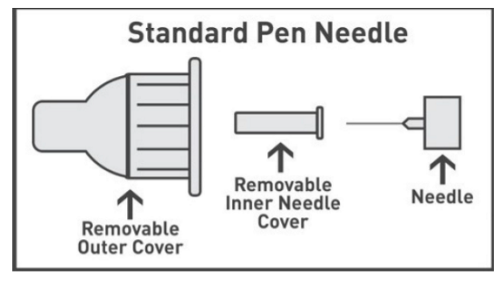
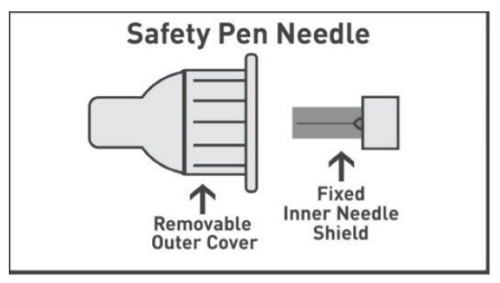
The NovoLog FlexPen uses either a standard needle or a safety needle. Use the type that you were trained to use.
Injection sites
NovoLog FlexPen is used to give an injection (shot) of NovoLog under the skin. This injection is given into the fatty areas of the body called injection sites.
The usual sites are:
- Stomach (abdomen)
- Upper thighs
- Back of upper arms
Rotate the injection sites each time so that the fat areas do not get irritated and scarred. Do not use the same site for each injection. Never inject NovoLog into a vein or muscle.
Air shots
You should do an air shot before each injection, after the needle is attached.
Performing an air shot helps you check that the insulin flow is good before you select and inject the dose. This way you can make sure that your child receives the full dose and avoid injecting air.
To do an air shot:
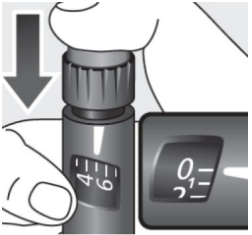
- Turn the dose selector to 2 units.
Selecting your child’s dose
Turn the dose selector to select the number of units you need to inject. The dose pointer should line up with your child’s dose.
Possible side effects
Early side effects may include:
- Itching or rash at the injection site.
- Skin thickening or pits at the injection site
- Allergic reactions
Later side effects may include:
- Low blood sugar (hypoglycemia)
- Skin rash, itching
- Weight gain
These are the most common side effects, but there may be others. Please report all side effects to the doctor or nurse.
In case of a severe side effect or reaction, call your doctor, nurse, or pharmacist at 901-595-3300. If you are outside the Memphis area, dial toll-free 1-866-278-5833, and press 0 once the call is connected.
Low blood sugar
Know the signs of low blood sugar. Young children may not understand the signs of low blood sugar.
Common signs of low blood sugar are:
- Anxiety
- Confusion
- Feeling irritable
- Headache
- Mood changes
- Shaking
- Feeling dizzy
- Fast heartbeat
- Sweating
- Feeling tired
If your child has any of these signs, check the blood sugar right away.
If the blood sugar is less than 70 mg/dL, give your child a quick source of sugar. Always carry some type of quick sugar source with you.
Check your child’s blood sugar 15 minutes after treating the low blood sugar. If the blood sugar is less than 70mg/dL the second time, treat again and call your child’s doctor. Once the blood sugar is above 70mg/dL, your child needs to eat a snack containing protein.
Quick sources of sugar to treat low blood sugar include:
- Glucose tablets
- Juice
- Regular soda (not sugar-free)
- Raisins
- Saltine crackers
- Sugar or corn syrup
- Cake frosting
Do not use chocolate, cookies or cake to treat low blood sugar. These foods have lots of sugar but are high in fat, which makes them slower at boosting your child’s blood sugar.
Contact the doctor right away or go to the hospital in these cases:
- Low blood sugar happens again
- You cannot fix the low blood sugar
- Your child has a seizure
- Your child passes out
- Your child is not feeling better in 2–3 days or is feeling worse
Questions?
If you have questions or concerns, please call 901-595-3300 and ask for your child’s primary clinic. If you are calling after hours or on the weekend, ask for the nursing coordinator. If you are outside the Memphis area, dial toll-free 1-866-278-5833.