The Levemir® (LEV-uh-mere) FlexTouch® allows you to give your child insulin without having to get the medicine out of a vial with a separate syringe.
Levemir FlexTouch contains insulin detemir, also called Levemir, which is a long-acting insulin
- It is used to help patients with high blood sugar levels.
- It can provide blood sugar control for up to 24 hours.
- It is a clear, colorless liquid that is injected under the skin.
The Levemir FlexTouch is often called a Levemir FlexTouch pen, because it looks like a pen and can be carried in your pocket or purse.
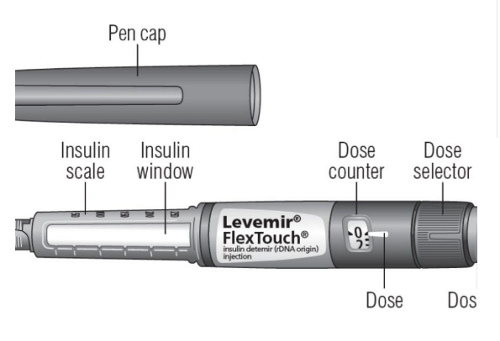
The Levemir FlexTouch pen
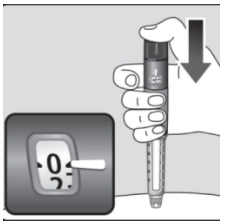
The Levemir FlexTouch pen is a prefilled disposable device. It contains 300 units of U-100 Levemir. It uses a built-in spring mechanism to inject the insulin. The push button does not extend and requires a small amount of force to inject a dose. When your child’s dose is delivered, you should hear an audible click letting you know that the full dose has been received.
The pen can deliver doses from 1 to 80 units in a single injection. The large dose display shows the number of units you have selected to give as a dose.
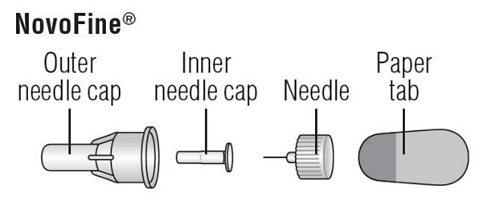
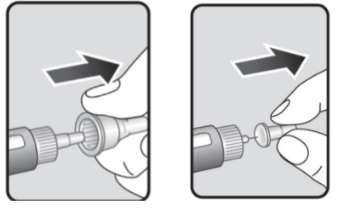
Needles for the Levemir FlexTouch pen
You will receive needles made specifically for the Levemir FlexTouch pen. These are called NovoFine® needles.
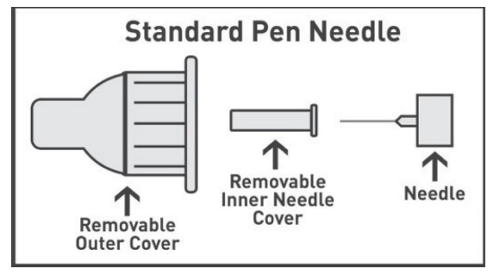
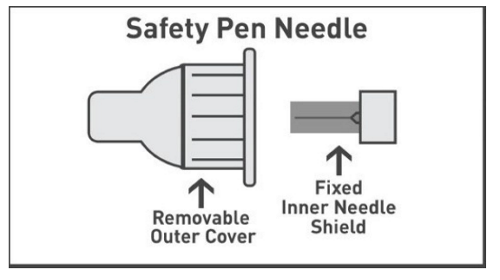
The Levemir FlexTouch pen uses either a standard needle or a safety needle. Use the type that you were trained to use.
Injection sites
The Levemir FlexTouch pen is used to give an injection (shot) of Levemir under the skin. This injection is given into the fatty areas of the body called injection sites.
The usual sites are:
- Stomach (abdomen)
- Upper thighs
- Back of upper arms
Rotate the injection sites each time so that the fat areas do not get irritated and scarred. Do not use the same site for each injection.
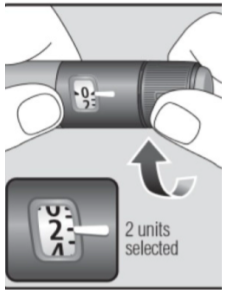
Selecting your child’s dose
Turn the dose selector to select the number of units you need to inject. The dose pointer should line up with your child’s dose.
If you select the wrong dose, you can turn the dose selector forward or backward to correct the dose.
- The even numbers are printed on the dial.
- The odd numbers are shown as lines.
Possible side effects
Early side effects may include:
- Itching or rash at the injection site.
- Skin thickening or pits at the injection site
- Allergic reactions
Later side effects may include:
- Low blood sugar (hypoglycemia)
- Skin rash, itching
- Weight gain
These are the most common side effects, but there may be others. Please report all side effects to the doctor or nurse. In case of a severe side effect or reaction, call your doctor, nurse, or pharmacist at 901-595-3300. If you are outside the Memphis area, dial toll-free 1-866-278-5833, and press 0 once the call is connected.
Low blood sugar
Know the signs of low blood sugar. Young children may not understand the signs of low blood sugar.
If your child has any of these signs, check the blood sugar right away.
If the blood sugar is less than 70 mg/dL, give your child a quick source of sugar. Always carry some type of quick sugar source with you.
Check your child’s blood sugar 15 minutes after treating the low blood sugar. If the blood sugar is less than 70mg/dL the second time, treat again and call your child’s doctor. Once the blood sugar is above 70mg/dL, your child needs to eat a snack containing protein.
Quick sources of sugar to treat low blood sugar include:
- Glucose tablets
- Juice
- Regular soda (not sugar-free)
- Raisins
- Saltine crackers
- Sugar or corn syrup
- Cake frosting
Do not use chocolate, cookies or cake to treat low blood sugar. These foods have lots of sugar but are high in fat, which makes them slower at boosting your child’s blood sugar.
Contact the doctor right away or go to the hospital in these cases:
- Low blood sugar happens again
- You cannot fix low blood sugar
- Your child has a seizure
- Your child passes out
- Your child is not feeling better in 2–3 days or is feeling worse
Questions?
If you have questions or concerns, please call 901-595-3300 and ask for your child’s primary clinic. If you are calling after hours or on the weekend, ask for the nursing coordinator. If you are outside the Memphis area, dial toll-free 1-866-278-5833.